The $21,981 Spread: How a program for the poor became a $54 billion wealth transfer.
Dynasty 5: The 340B Empires: The Safety-Net Exploiters | Five Dynasties Finale
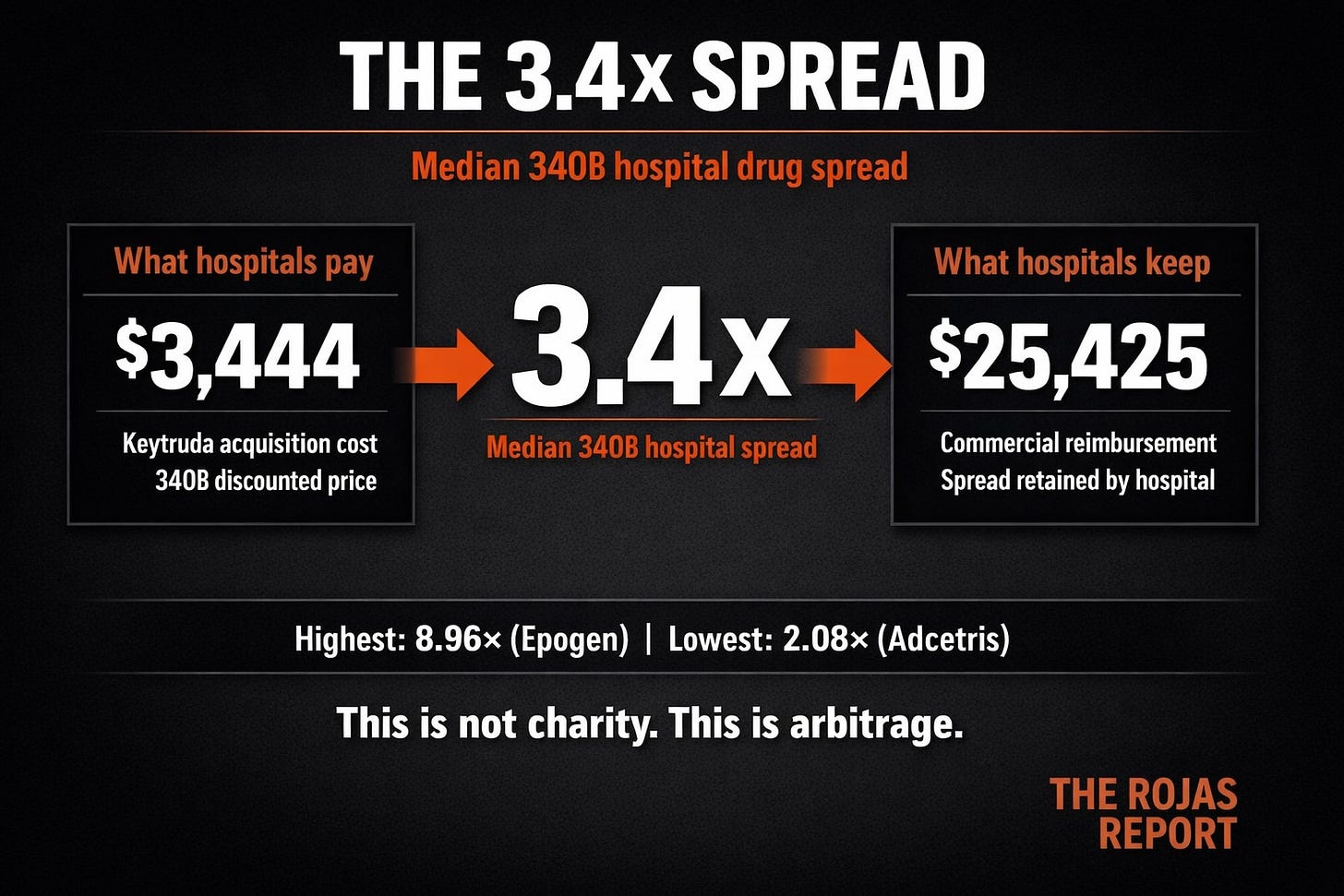
Your hospital bought a cancer drug for $3,444.
They collected $25,425 from your insurance coverage.
$21,981 spread. One dose.
It’s called 340B.
And you’ve never heard of it.
In 1992, Congress created a program to help the poorest hospitals in America afford prescription drugs.
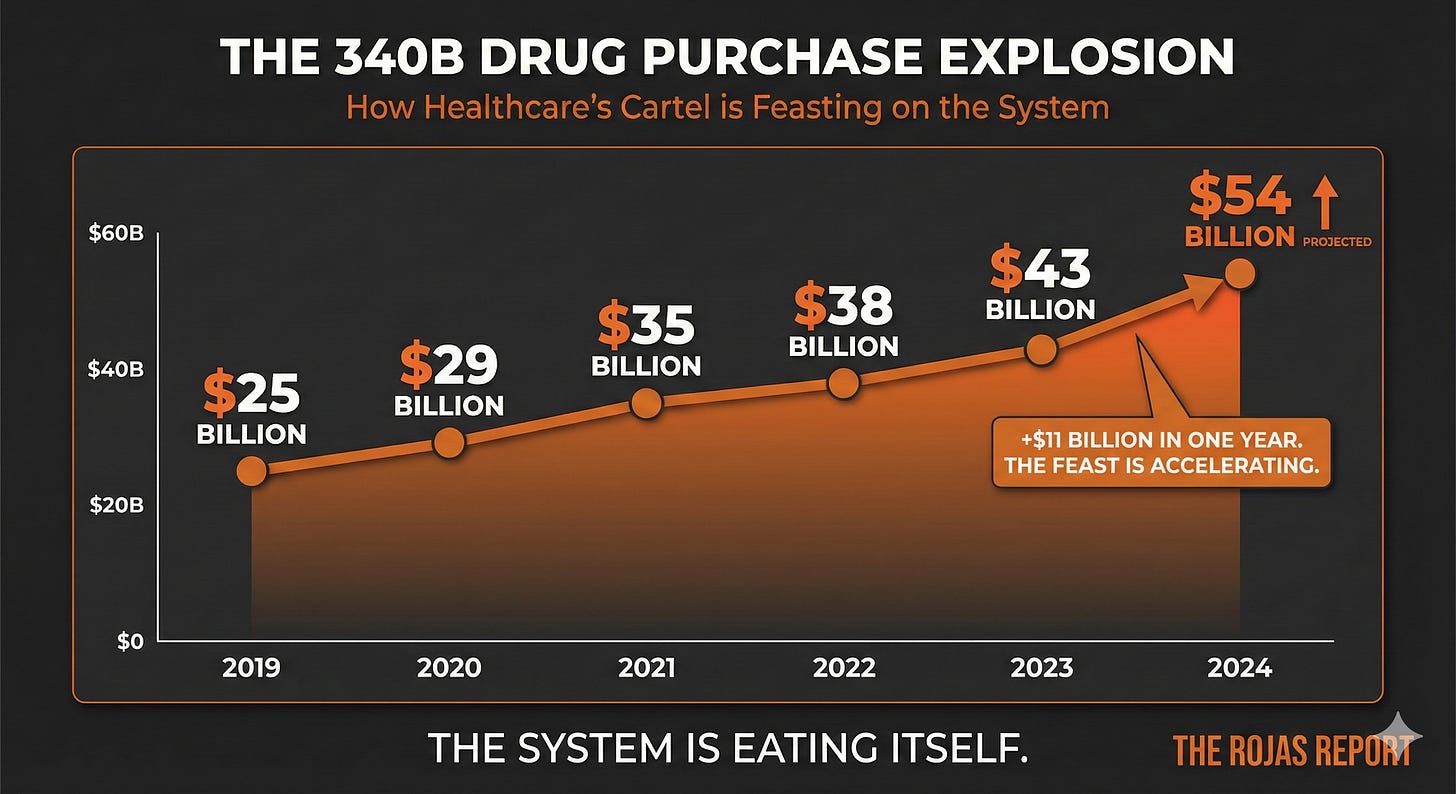
Thirty-three years later, that program has become a $54 billion annual spread trade.
340B hospitals keep 3.4 times what they paid for drugs.
They spend 1% of their operating costs on charity care.
That’s not a bug.
That’s 340B working exactly as the hospitals designed it to work.
The Spread Trade
Here’s how 340B works:
Drug manufacturers must sell outpatient medications to qualifying hospitals at steep discounts, typically 25% to 50% below list price.
The hospital buys the drug at 340B pricing. Bills the insurer or patient at full price. Pockets the difference.
Let me show you what that looks like.
Keytruda, the blockbuster cancer immunotherapy.
340B acquisition cost: $3,444
What the hospital keeps from your insurer: $25,425
Spread: $21,981
Per dose!!!!
A 2024 Community Oncology Alliance study analyzed what 340B hospitals actually keep on drug reimbursements. They obtained pricing data from 49 hospitals that actually complied with transparency requirements.
The finding:
340B hospitals keep 3.4 times their acquisition cost.
The highest markup? 8.96 times, Epogen.
The lowest? 2.08 times, Adcetris.
Even the lowest 340B spread means hospitals collect 108% more than acquisition cost on drugs intended for low-income patients.
The Growth Machine
The 340B program was tiny when it started.
A few hundred safety-net hospitals.
A billion dollars in drug purchases.
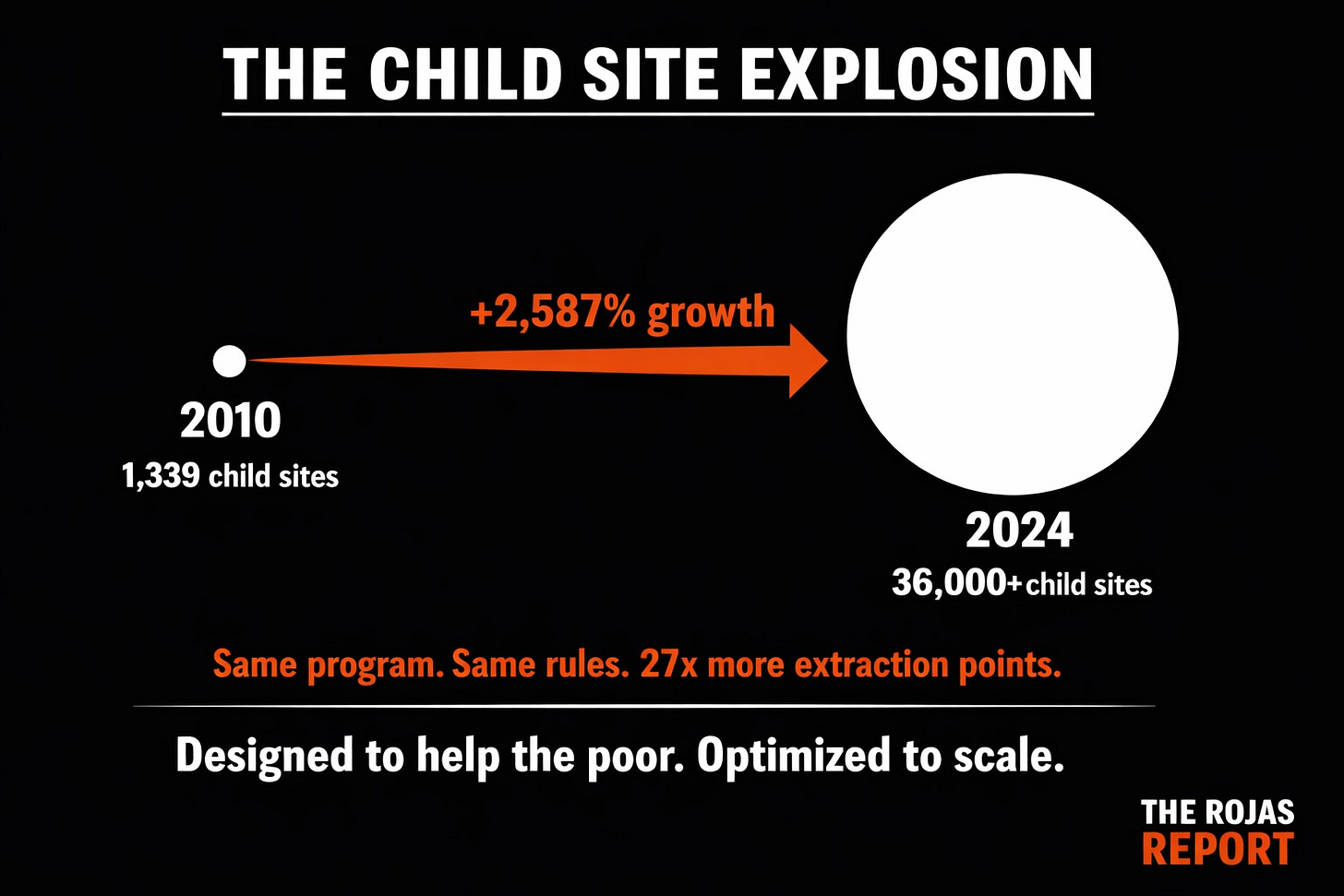
Then came 2010.
HRSA issued new guidance allowing any covered entity to use unlimited contract pharmacies. Any affiliated outpatient site could be registered as a child site for 340B pricing.
The floodgates opened.
Child sites: from 1,339 in 2010 to over 36,000 today.
Contract pharmacy locations: 33,000+ — that’s half of all U.S. pharmacies.
The safety-net program is now one of the most extensive drug purchasing programs in America.
The Oncology Play
Here’s why hospitals acquired your oncologist.
A single oncologist in a 340B-eligible hospital can generate $1 million+ in annual 340B profit.
So they bought.
The 2018 NEJM study found 340B hospitals employ 230% more oncologists than similar non-340B hospitals.
But here’s the catch: those 340B hospitals were serving a lower proportion of low-income patients than before.
They weren’t buying practices to serve people experiencing poverty. They were buying practices because the spread was too lucrative to ignore.
The Community Oncology Alliance has tracked the carnage:
1,750 community oncology practices closed, acquired, or in financial distress since 2008
80%+ of those acquisitions went to 340B hospitals
Hospital acquisitions increased 9.7% in years with expanding 340B provisions
When Methodist Le Bonheur acquired West Cancer Clinic in Memphis, they generated $50 million in 340B profit in a single year.
When Duke acquired its oncology network, the hospital netted $69.7 million in one year — bought $65.8 million in drugs, billed insurers $135.5 million.
One acquisition. One year. $70 million in spread.
The Bon Secours Scandal
In 2022, The New York Times exposed what was happening at Bon Secours Mercy Health’s Richmond Community Hospital.
Richmond Community qualified for 340B because it served a disproportionate share of poor and uninsured patients in one of the poorest neighborhoods in Virginia.
What Bon Secours did with that designation:
Extracted $276 million in 340B revenue over five years
Posted $100 million in annual profit margin
Opened suburban cancer clinics in wealthy neighborhoods — registered as “child sites” of Richmond Community
Charged insurers full price for drugs acquired at 340B discounts
Meanwhile, at the actual Richmond Community Hospital:
Cut services
Reduced bed capacity
Neglected the facility
The census tract around the hospital had an 81% higher COVID death rate than the city average
When asked how they spent their 340B revenue, Bon Secours told Senate investigators:
“It goes into general revenue. We don’t specifically track it.”
Same answer from Cleveland Clinic.
Same answer from every system that’s ever been asked.
The Transparency Failure
In 2021, CMS finalized hospital price transparency rules requiring hospitals to publish their negotiated prices.
The Community Oncology Alliance set out to assess 340B hospital compliance.
Out of 1,000+ 340B DSH hospitals:
Only 352 attempted to comply
Only 49 published individual negotiated payer price data for drugs
The rest? They didn’t bother.
And no one made them.
Those 49 hospitals, less than 5%, served as the sole basis for understanding what 340B hospitals actually charge. The other 95% operate in complete darkness.
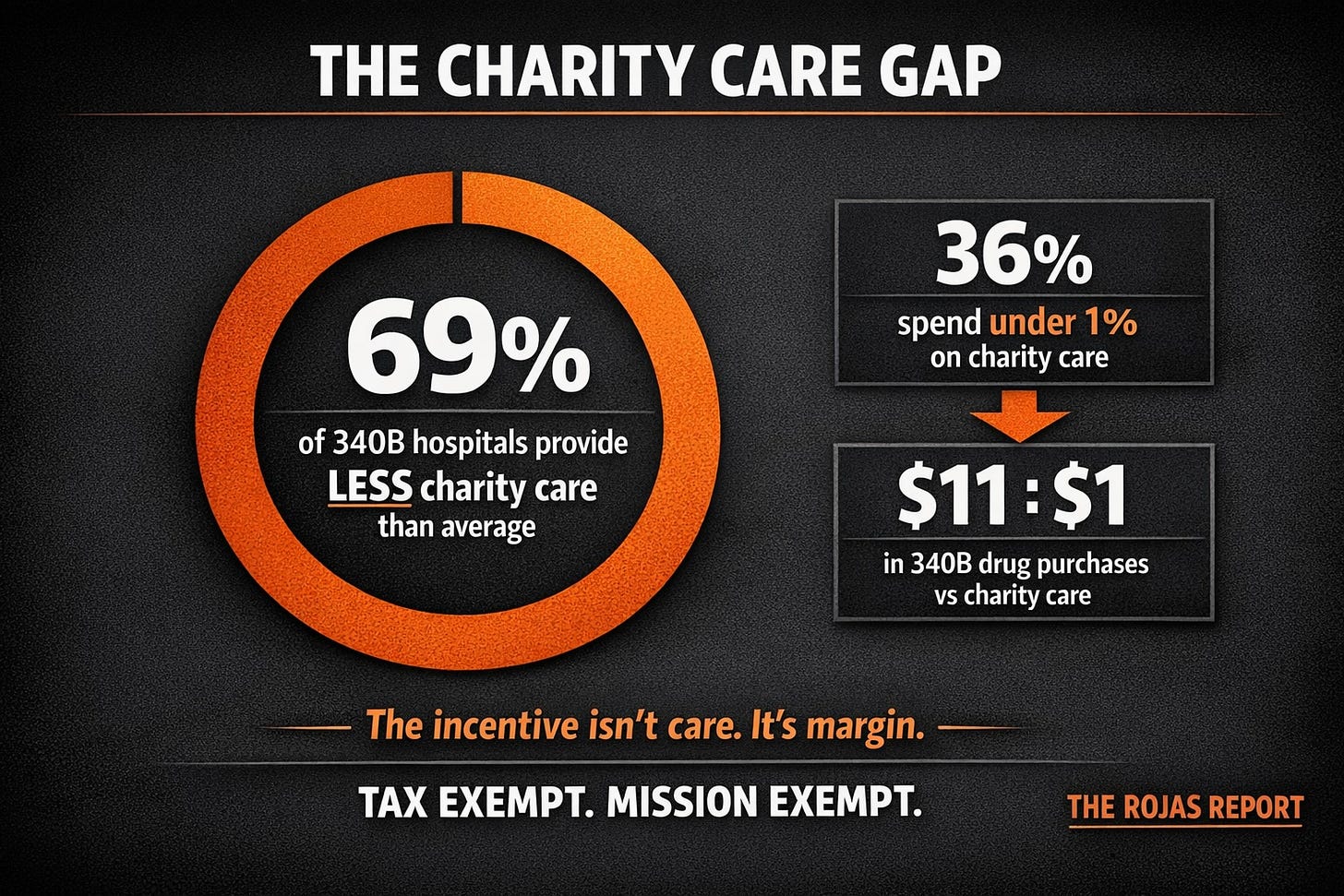
The Charity Care Gap
The Lown Institute studied 340B hospital charity care:
69% of 340B hospitals provided less charity care than the national average
36% spent under 1% of expenses on charity care
The hospitals receiving the largest 340B discounts showed no correlation with higher charity care
The Government Accountability Office testified to Congress in November 2024:
Most 340B oversight recommendations remain unimplemented
HRSA lacks enforcement authority
No hospital has ever lost 340B eligibility for failing to serve the poor
A 2020 study found the ratio:
For every $1 increase in charity care, 340B hospitals increased their 340B purchases by $11.
The program isn’t funding charity.
It’s funding acquisitions.
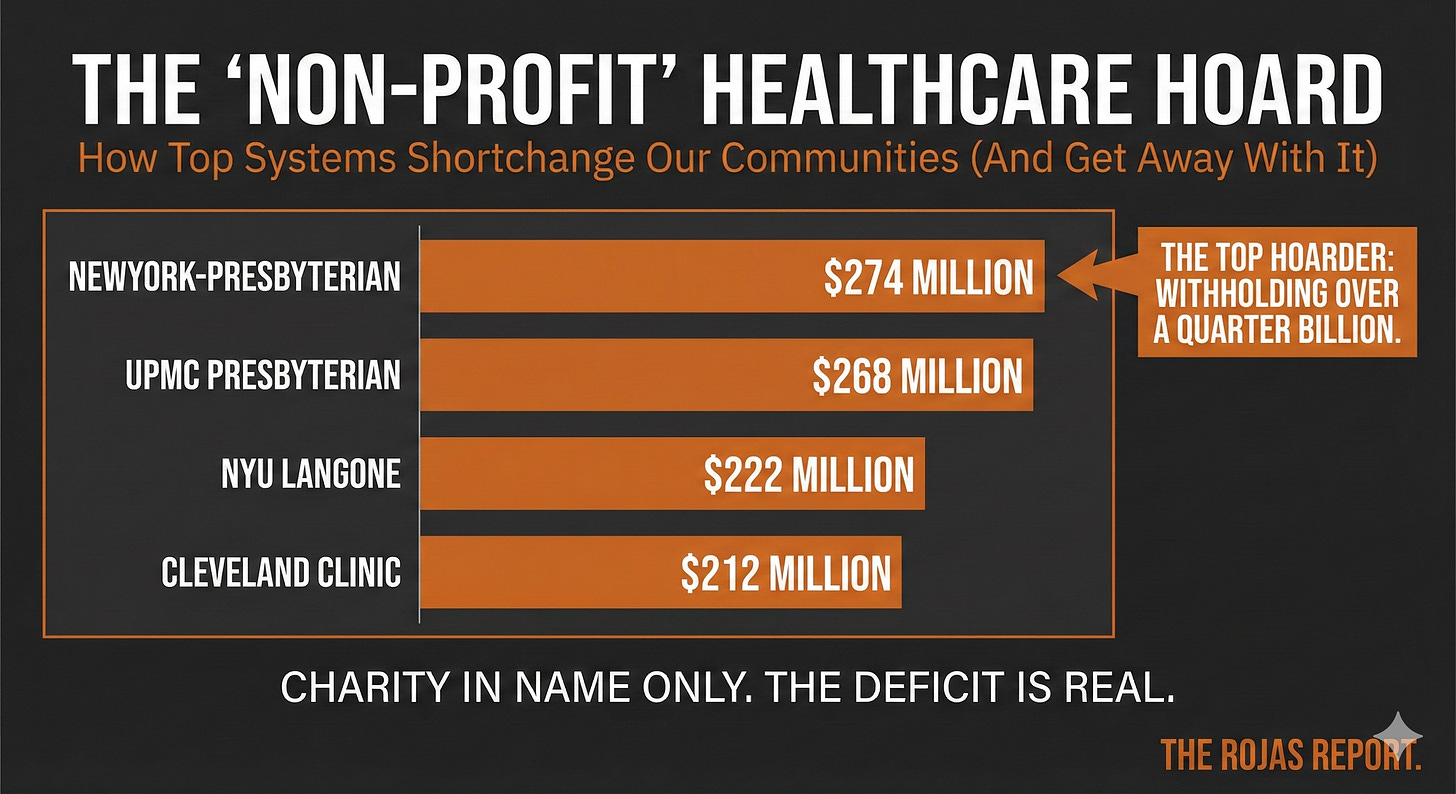
The Fair Share Deficit
The Lown Institute calculates a “fair share deficit” — the gap between what hospitals receive in tax exemptions and subsidies versus what they provide in charity care.
The largest 340B hospitals have some of the largest deficits:
These are among the wealthiest hospital systems in America. They qualify for 340B. They pay no taxes. They provide less charity care than they take in exemptions.
And they lobby furiously to keep it that way.
The Moats Stack
This is where the Five Dynasties converge.
Kaiser proved you could own both the insurance and the care.
Their 340B-eligible facilities capture spreads on both sides of the transaction.
Academic Medical Centers: Hopkins, Penn, Duke, Cleveland Clinic, layer 340B on top of GME funding, NIH grants, and CON protection. They’re untouchable.
Catholic Systems: CommonSpirit, Ascension, Providence, Trinity, Bon Secours, use 340B to fund cross-market acquisitions the FTC can’t challenge. The Richmond scandal was a Catholic system.
Regional Monopolies: UPMC, Sutter, Intermountain, Advocate, own beds, own health plans, AND capture 340B spreads. Triple extraction.
Every Dynasty uses 340B.
Every Dynasty stacks it on top of their other moats.
CON laws block competition.
Tax exemptions eliminate the burden.
Facility fees are extracted from every visit.
GME funds the training pipeline.
340B funds the acquisitions.
The moats stack.
The Pattern Is the Point
340B was a noble idea: Help poor hospitals afford drugs so they can serve poor patients.
But there were no guardrails.
No accountability.
No transparency.
The hospitals saw an arbitrage opportunity and took it.
The oncology practices in wealthy suburbs?
Acquired and converted to 340B child sites.
The independent physicians?
Bought out or driven out.
The contract pharmacy market?
Captured by CVS, Walgreens, and the PBMs.
The safety-net patients the program was designed to help? The hospitals that qualify based on serving them strip resources from those very facilities to fund expansion elsewhere.
Same pattern as Certificate of Need.
Same pattern as facility fees.
Same pattern as tax exemption.
Same pattern as the physician ownership ban.
Write a rule to help the vulnerable. Watch the powerful capture it.
What Reform Would Look Like
Transparency first. Require hospitals to report exactly how much 340B revenue they generate and how it’s spent. Make it public. The 95% hiding in darkness need to be exposed.
Patient eligibility standards. Tie 340B discounts to actual care for low-income patients, not just hospital designation.
Child site restrictions. Require child sites to serve similar patient populations as the qualifying hospital. No more suburban oncology clinics piggybacking on inner-city DSH designations.
Charity care minimums. If you’re going to extract billions from a program designed for the poor, prove you’re actually serving them.
Contract pharmacy limits. The unlimited contract pharmacy guidance of 2010 opened the floodgates. Close them.
None of this will happen easily.
The hospitals will fight.
The lobbying will be fierce.
Senator Cassidy just released findings from a years-long congressional probe.
The GAO has testified repeatedly.
The data is overwhelming.
But the program can’t keep growing at 24.5% annually while the patients it was designed to serve get worse care.
The Fifth Dynasty
The 340B Empires are the most subtle of the Five Dynasties.
Kaiser is visible, everyone knows the model.
Academic Medical Centers have prestige, everyone knows the names.
Catholic Systems have the cross, everyone sees the branding.
Regional Monopolies have market power, everyone feels the prices.
But 340B? Most Americans have never heard of it.
A $54 billion program.
3.4x spreads.
1,750 oncology practices destroyed.
Zero transparency.
Zero accountability.
Hidden in plain sight.
That’s the Fifth Dynasty.
The Series Concludes
This week, we mapped the architecture of American healthcare’s protected class:
Day 1: Kaiser showed them that the integration works.
Day 2: Academic Medical Centers captured prestige, funding, and protection.
Day 3: Catholic Systems consolidated across markets the FTC couldn’t touch.
Day 4: Regional Monopolies proved you could own both the beds and the premiums.
Day 5: 340B Empires revealed how a safety-net program became an acquisition engine.
The Five Families, United, CVS, Elevance, Cigna, Centene, get the attention.
They’re publicly traded. They answer to shareholders. Their denials make the news.
But they didn’t build this system. They inherited it.
The Dynasties built the castle. The Families moved in.
This is the journalism the hospital lobby pays millions to suppress.
If you followed along with this series, if this hit different, do two things:
1. Subscribe. Paid subscribers fund investigations they can’t kill.
2. Gift this to everyone you know. Your brother-in-law at the hospital. Your cousin in insurance. Your neighbor who just got a surprise bill. This is the Christmas gift that explains why their premiums went up 18% again.
Share the truth. Subscribe. Let’s go.
KEY STATISTICS REFERENCE
Program Size (2024 — IQVIA)
$54 billion — Total 340B purchases (WAC dollars)
24.5% — Year-over-year growth
118.6% — Five-year growth (2019-2024)
3x — 340B growth rate vs. non-340B drug sales
What Hospitals Keep (COA 2024)
3.4x — Median multiple of acquisition cost kept
8.96x — Highest (Epogen)
2.08x — Lowest (Adcetris)
49 — Hospitals that actually published drug pricing data
Hospital Margins (JAMA 2024)
76% — Share of reimbursement 340B hospitals kept
53% — Share of reimbursement non-340B hospitals kept
23 points — 340B margin advantage
Program Growth
1,339 → 36,000+ — Child site explosion (2010-2024)
33,000+ — Contract pharmacy locations
53,000+ — Total care sites affiliated with 340B entities
Oncology Impact
$1 million+ — Annual 340B profit per oncologist
230% — More oncologists at 340B hospitals (NEJM)
1,750 — Community practices closed/acquired/struggling since 2008
80%+ — Acquisitions went to 340B hospitals
Bon Secours Case Study
$276 million — 340B revenue over 5 years
$100 million — Annual profit margin
81% — Higher COVID death rate in hospital census tract
$21,981 — Keytruda spread per dose
Charity Care Gap
69% — 340B hospitals below the national charity care average
36% — Spent under 1% on charity care
$11:$1 — Ratio of 340B increase to charity care increase
0 — Hospitals that have lost 340B eligibility for failing the mission



Thank you, Dutch, for uncovering all this for your readers. Of course, all this is a travesty.
Are any of the noises MAHA, Trump, Congress, and HHS are making about healthcare and drug affordability even touching the five dynasties? Or are they simply nibbling around the edges and putting lipstick on a pig?
Have you been able to meet with anyone to present this information so real reform could happen?
This post is the perfect primer that the world needs to see.